Introduction: What is 340B?
The 340B drug pricing program was created by Congress in 1992 to provide certain health care providers significant discounts on prescription drugs. The program, which is administered by HRSA, allows eligible hospitals, clinics, pharmacies, nursing homes, home healthcare agencies, hospices, dialysis centers and long-term acute care facilities (among others) to replenish prescription inventories at prices far below market rates.
The purpose of 340B programs is to enable eligible providers to create higher margins on prescriptions as a means of filling revenue gaps that are inherent to their business models and patient populations.
The 340B program covers thousands of prescription medications. Many of the hospitals who take advantage of the program’s discounts save millions of dollars a year on their prescription costs. Savings and revenue which, for some of the hospitals VytlOne serves, literally make the difference between solvency and closure.
How two health systems use their 340B revenue
In a previous post, we profiled Directors Of Pharmacy at two health systems served by VytlOne’s 340B team: Southwest Mississippi Regional Medical Center’s Tiffany Poole and Conway [South Carolina] Medical Center’s Andrew Wright. Below are two excerpts from that post:
TIFFANY
Our facility is the only option for so many patients. We have to find a way to serve them, and that takes our finance team and our patient care team creating a balance. That's the whole reason Congress started 340B — to increase access to healthcare for everyone, and spread scarce resources in our most underserved communities. Our relationship with VytlOne lets us spread those scarce resources further than we ever could on our own.
ANDREW
It's allowed us to expand into areas of medicine we never thought we could offer. We've added a cancer center, a pain clinic as part of our orthopedic practice, a dermatology clinic, and a women's center. We’re expanding our footprint, and we’re treating so many more patients than we used-to. Without VytlOne and 340B, that wouldn't have been possible.
All of which begs the question: Why don’t all 340B-eligible hospitals and health systems take advantage of their legal rights to the program’s savings and discounts? In our experience, the primary reason (by far) is fear of the consequences of non-compliance — coupled with a lack of administrative bandwidth to effectively develop and administer 340B programs.
That’s why we’ve created this comprehensive guide: To give eligible entities all the information they need to understand the 340B program’s requirements — and how to 1) optimize their savings from 340B-elible medication replenishment and 2) improve patient care & satisfaction, while 3) still maintaining full compliance at all times.
The 340B landscape, and what it means for eligible entities in 2025
As we report in Chapter 7 of this resource guide, the 340B landscape continues to evolve rapidly, with ongoing 340B ESP and other manufacturer restrictions, new compliance hurdles, and increasing financial pressures on covered entities. Chief among those new challenges is HRSA’s Rebate Model Pilot Program, introduced July 31 — a program which, if expanded to include all 340B-eligible prescriptions, could literally have a catastrophic impact on every participating 340B health system’s finances, moving forward.
HRSA’s track record in enforcing the 340B law had already been marked by a series of very public failures. The agency has even admitted publicly that, for all practical purposes, it has no real power to enforce 340B program guidelines — an admission it made shortly after the U.S. House Appropriations Committee turned down its request for broad regulatory authority over the 340B program.
In Chapter 7 below, we also discuss Bausch Health's (BHC) decision to cease participation in the Medicaid Drug Rebate Program and the 340B Drug Pricing Program effective October 1, 2025.
To jump straight to Chapter 7 and our current 340B overview, updated November 2025, Click Here.
Table of Contents
Chapter 1: How do 340B programs work?
Chapter 2: What entities, patients and drugs are 340B-eligible?
Chapter 3: Optimizing savings and patient care through 340B
Chapter 4: Maintaining 340B compliance
Chapter 5: 340B ESP & manufacturer restrictions, and how to overcome them
Chapter 6: Using specialty pharmacy to optimize 340B revenue and patient outcomes
Chapter 7: 340B's outlook moving forward, and how to prepare your program
Chapter 1: How do 340B programs work?
When a patient receives a 340B-eligible prescription from an eligible entity, the entity is reimbursed for the full market price of the drugs, but pays only a fraction of the drugs’ cost — by replenishing the medication from the 340B catalog.
Who pays the 340B costs?
Manufacturers bear the burden of the cost and reimburse wholesalers for 340B discounts on 340B-eligible medications.
How does the 340B payment process work?
As a covered entity, you send your encounter (visit) data to your TPA, and your pharmacy sends the TPA the prescription data. Your TPA creates a match when it determines that 340B qualification criteria has been met, and your pharmacy then orders from your 340B account to replenish the drugs.
Clients served by VytlOne use a proprietary software system, which monitors every prescription their organizations fill, and identifies every eligible prescription generating sufficient savings to justify the time and effort to claim 340B savings. This extra layer of monitoring improves compliance, while hunting-down hidden opportunities for more 340B savings.
VytlOne works with each client to determine how aggressively they want to pursue 340B savings. We then maintain comprehensive records on every prescription applied for — always assuring clients of complete compliance.
Which pharmacies can I use for 340B prescriptions?
340B-eligible hospitals can use the in-house (or on-campus) retail pharmacies they own and manage, as well as “contract pharmacies” — which can be both on-campus and off.
You can extend 340B eligibility to contract pharmacies (onsite or off) if they meet HRSA’s requirements — which include the following: Your contract pharmacies must 1) register for the 340B Program, 2) be listed on the 340B OPAIS prior to dispensing 340B drugs on your behalf, 3) not use 340B drugs for Medicaid patients unless you have an arrangement in place with the state.
Covered entities often choose contract pharmacies to dispense 340B drugs to patients for a number of reasons. Many hospitals, for instance, prefer their on-campus retail pharmacies to be operated independently. Some hospitals reach contract pharmacy agreements with multiple pharmacies in their communities, offering their patients more convenience, access and options when filling prescriptions written by their providers.
SIMPLIFIED PAYMENT PROCESS*
(No Manufacturer Restrictions)
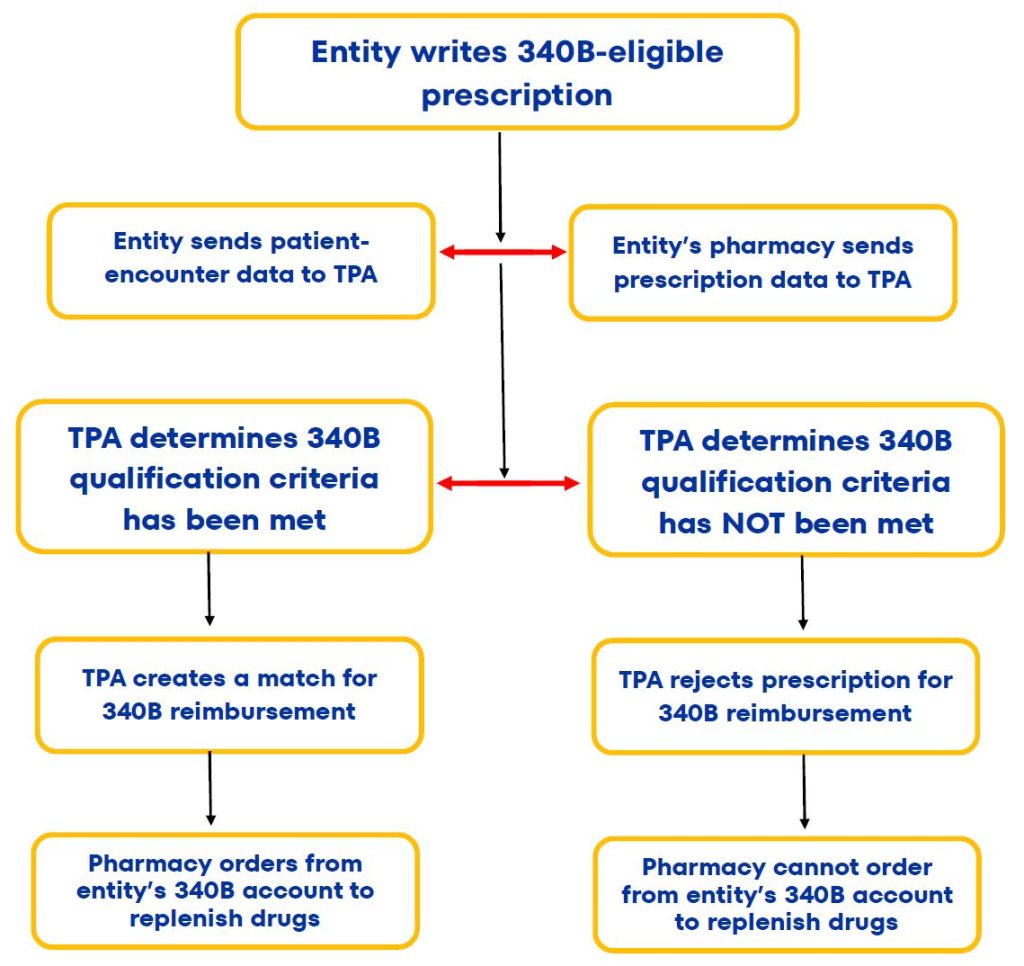
*NOTE
The TPA steps described above are for off-site contract pharmacies, but aren't necessary for health systems' on-campus pharmacies.

What Are The Requirements For 340B Programs?
Covered entities must meet the following ongoing requirements:
- Keep 340B OPAIS information accurate and up to date.
- Register new outpatient facilities and contract pharmacies as they are added.
- Prevent diversion to ineligible patients.
- Maintain auditable records documenting compliance with 340B Program requirements.
As a covered entity, it’s also your responsibility to notify drug manufacturers and wholesalers that you plan to purchase drugs at 340B prices. The wholesalers and manufacturers verify your enrollment on the 340B database and must sell their drugs to you — at or below the maximum price determined under the 340B statute.
How do I enroll in the 340B program?
To register, you need a 340B Office of Pharmacy Affairs (340B OPAIS) user account. To get started, visit the 340B OPAIS Registration page, and select the appropriate link toward the bottom of the page — either Grantee Registration or Hospital Registration.
The system should run you through the process from there. It’s important to know, in advance, that you must complete your registration in a single session. Which is why you’ll need to have your latest filed Medicare cost report on-hand while you’re completing the process.
You’ll also you’ll need to enroll your main location first, then add any Child Sites.
What is a 340B Child Site?
HRSA defines a 340B Child Site as an off-site outpatient clinic or location that uses, or purchases, 340B drugs for its patients. In general, “off-site” means a location has a separate physical address than the hospital parent site, and is not located within the main hospital.
Can my TPA apply for 340B discounts on my behalf?
Yes. However, the work performed by TPAs has emerged as a distinct risk to Covered Entities — a topic we’ll cover, in-depth, in Chapter 3.
NOTE: VytlOne is not a TPA. However, we work closely with our clients’ TPAs, holding them accountable and ensuring that they maintain the same standards for 340B compliance that we do. To learn more about how VytlOne optimizes 340B savings and revenue, visit this page of our website.
How do 340B programs interact with the MDRP?
The Medicaid rebate program interacts with other programs receiving manufacturer discounts on drugs. As a condition of participation in the Medicaid Drug Rebate program, manufacturers must also participate in the 340B drug-discount program.
340B ceiling prices are calculated to match Medicaid prices, but manufacturers can (but rarely do) provide additional discounts to 340B providers that are not subject to the best price rule.
Safety net providers eligible for 340B discounts can choose whether or not they provide drugs purchased with the program discounts to Medicaid beneficiaries within state guidelines. This may not include drugs paid for by managed-care plans or those dispensed at contract pharmacies, but MCOs also are required to exclude 340B claims from reports they provide to states for rebate purposes.
WANT OUR RESOURCE GUIDE
IN DOWNLOADABLE PDF?
Chapter 2: What entities, patients and drugs are 340B-eligible?
The following hospital categories are eligible for 340B participation
- Disproportionate Share Hospitals (DSH)
- Sole Community Hospitals (SCH)
- Rural Referral Centers (RRC)
- Critical Access Hospitals (CAH)
- Children’s Hospitals (PED)
- Free-Standing Cancer Hospitals (CAN)
340B eligibility requirements: An overview
In order for hospitals to qualify for the 340B program, they must meet the three requirements below — unless they are Rural Hospitals; in which case, they must meet only the first two requirements.
- Government owned or government-controlled.
In other words, hospitals must be either A) Owned or operated by a state or local government, B) Public or private non-profit corporations which have been formally granted governmental powers by their state or local government, OR C) Private non-profit hospitals under contract with their state or local governments to provide health care services to low-income patients who are not entitled to Medicare or Medicaid benefits. - Disproportionate Share Hospitals.
Disproportionate Share Hospitals must have an adjustment percentage (or the percentage by which the hospital’s allowable operating costs of inpatient hospital services exceeds the hospital’s target amount) higher than 11.75% for the most recent cost reporting period ending before the calendar quarter involved. Sole Community Hospitals and Rural Referral Centers must have an adjustment percentage of greater than 8 percent.Free-standing children’s hospitals and free-standing cancer hospitals must have a payer mix that gives them a DSH percentage of greater than 11.75 percent. Critical Access Hospitals do not have a DSH adjustment percentage requirement.NOTE: A hospital’s DSH adjustment depends on the number of inpatient days of its Medicaid and Supplemental Security Income (SSI) patients. - DSH hospitals, children’s hospitals and free-standing cancer hospitals meeting the first two criteria.
These hospitals are eligible to participate in the 340B program if they do not obtain covered outpatient drugs through Group Purchasing Organizations (GPOs), or through other group purchasing arrangements. At the same time, hospitals participating in 340B as CAHs, RRCs and SCHs are not subject to the GPO prohibition.
The following types of facilities are included in the 340B program
- Freestanding acute care general hospitals
- Psychiatric hospitals
- Long term/continuing care nursing homes
- Home infusion therapy centers
- Hospices
- Federally qualified health centers
- Rural health clinics
- State mental institutions
- Indian Health Service facilities
- Federally Qualified Health Centers
- Community-based rehabilitation programs.

Does HRSA Allow 340B Child Sites?
Yes. OPA requires that a covered entity register, as child sites, all offsite clinics, departments and services where 340B drugs are purchased or used, whether or not they are in the entity’s primary campus.
“Offsite” generally means a location has a separate physical address than the hospital parent site. A hospital does not need to register outpatient clinics, departments or services located within the entity's main hospital — but may do so if they appear on a reimbursable line of a hospital's most recently-filed cost report.
Applicable hospitals should ensure that their policies and procedures address qualification of 340B drugs dispensed at Child Sites for services not yet included in the most recently filed Medicare cost report, based on whether those locations meet Medicare provider-based requirements, whether the 340B covered entity maintains the responsibility and records of the patient's care, and whether the health care professionals prescribing 340B drugs have relationship with the 340B covered entity.

Which patients are covered under 340B programs?
Covered entities can dispense 340B-eligible prescriptions to patients who (1) Have established relationships with the covered entity, such that the entity maintains records of the patient's care; (2) Receive care from a professional employed by the covered entity, or under contract or other arrangements (e.g., referral for consultation) with the covered entity, such that responsibility for the care remains with the covered entity; and (3) Receive health services from the covered entity that are consistent with the services for which grant funding has been provided to the entity.
Under these guidelines, an individual is not considered a covered entity’s patient if the only health care service received by the patient from the entity is the dispensing of a drug for subsequent self-administration — or administration in the home setting.
Are 340B prices available for inpatient prescriptions?
No. 340B pricing applies to covered outpatient prescriptions only. Covered entities must therefore maintain appropriate tracking systems to ensure that covered outpatient drugs purchased through the 340B Program are not used for hospital inpatients — and it is the responsibility of health systems in the program to ensure that appropriate safeguards are in place to prevent these diversions.
What prescription drugs are eligible for 340B Savings?
In general, 340B eligibility involves both prescription medications and the covered entity writing the prescriptions. Here’s a simple checklist for determining whether drugs are eligible.
- As a covered entity, you have a relationship with the patient and maintains records of care.
- The services are provided by a healthcare professional who is either employed by, or contracted with, you.
- The responsibility for care rests with you, the covered entity.
- The services are within the scope of project for grantees and designees.
- The service provided must be more than just dispensing medication.
- The drug is administered in an eligible outpatient location or dispensed by one of your 340B contract pharmacies.
General drug exceptions to 340B eligibility
There are a few 340B-eligibility exceptions. These include vaccines and Orphan Drugs (which are, by definition, medications specifically developed to treat rare diseases or conditions — and drugs that have only recently been granted New Drug Status by the FDA).
Eligible drugs frequently NOT submitted for 340B savings
While narcotic medications are included among 340B eligible drugs, covered entities often choose to exclude them from their programs — due, primarily, to the complexity of procuring these medications for replenishment. That procurement complexity adds-up to significant time-and-effort costs. And as we’ve noted in a previous post, there’s no point in utilizing 340B discounts for medications when the time-and-effort costs exceed the savings generated.
About 340B Orphan Drugs
For the following covered entities, 340B-covered drugs do not include any drugs designated by the Secretary under Section 526 of the Federal Food, Drug, and Cosmetic Act for rare diseases and conditions:
- Free-standing cancer hospitals
- Rural referral centers
- Sole community hospitals
- Critical access hospitals
WANT OUR RESOURCE GUIDE
IN DOWNLOADABLE PDF?
Chapter 3: Optimizing savings and patient care through 340B
Why 340B programs should be optimized, and not maximized
For the health systems VytlOne serves, we pursue a policy of optimizing 340B savings that’s both aggressive and conservative. In other words, we believe you should aggressively pursue 340B savings for every prescription that’s worth pursuing. As we intimated earlier, some prescriptions are simply too low-cost, at market rates, to justify the effort needed to generate nominal savings.
Ideally optimized 340B programs generate a net savings on every eligible prescription claimed.
In our experience, 340B programs can’t be optimized without using proprietary software that keeps detailed electronic records on every prescription that hospitals' outpatient pharmacies (and contract pharmacies) fill, and enables them to easily and instantly produce all the evidence they would ever need to respond to audit requests.
Two key elements of optimized 340B programs
An unblemished record of performance
Whether 340B programs are managed entirely in-house, or they use outsourced partners for support, they should be managed by people with the skillsets — and, ideally, the track records — to ensure that compliance at all times. It’s worth noting that, since 2013, VytlOne has optimized dozens of 340B programs, and not once has a hospital we serve ever been fined for a 340B violation.
The ability to mine your records for 340B-eligible prescriptions: Present and Past.
VytlOne's proprietary software not only identifies current and past reimbursable prescriptions for our new clients, it automatically applies for those reimbursements. Typically, we’ll mine new clients’ prescriptions written up to one year prior to the date we started our service for them.
Get the most from your contract pharmacies
Contract pharmacies are critically important for optimizing the savings and revenue that your health system can generate with well-managed 340B programs. They’re also an important extension of your overall care of, and for, your outpatients. Increasing the number of independent pharmacies serving as contract pharmacies enhances your ability to offer your outpatients options and convenience in filing their prescriptions.
While you can’t steer patients toward specific pharmacies, you can certainly make your patients aware of the options available to them. Which is why maximizing the number of 340B contract pharmacies in a network should also maximize prescription-replenishment savings and revenue for eligible hospitals; at least in theory. In practice, we’ve found that to be far from the case.
Why do hospitals use 340B contract pharmacies?
In addition to the locational convenience health systems offer their outpatients by having multiple off-site pharmacies, many prefer their on-campus retail pharmacies to be independently owned and operated.
At the same time, community pharmacies need incentives to serve as contract pharmacies — and that’s where the problem lies with many contract pharmacy relationships.
Some contract pharmacies cost hospitals more (in fees) than they generate in 340B savings and revenue. What’s more, it’s often not for lack of prescription volume, but rather because those pharmacies simply won’t qualify many 340B-eligible medications. The other problem with many contract pharmacies is that they’re located too far from hospitals, and their patients, to offer them convenience in refilling their prescriptions.
We recognize that the goal of serving a community’s needs (even at a loss) often outweighs your hospital’s objective of maintaining only net-positive 340B contract pharmacy relationships. At the same time, we’ve helped a significant number of health systems replace contract pharmacies with low 340B match rates, with nearby pharmacies that have much higher match rates — generating far better 340B savings for those hospitals.
Optimizing the quality and number of your 340B eligible contract pharmacies
The simple truth is, we’ve never served (or seen) a 340B health system with adequate in-house resources to do just that. The typical number of quality 340B contract pharmacies we’ve added to the networks of health systems we serve is five to ten. For the network of one health system in South Carolina, we added nearly thirty contract pharmacies in just two years.
The challenge of building a contract pharmacy network
As any experienced professional will tell you, “sales” (for lack of a better term) ultimately comes-down to the number of calls you make. And in truth, that’s partly how we’ve done it for the health systems we serve. Everyone on our 340B team is trained to make inquiry calls to prospective contract pharmacies. What’s more, we make those calls armed with reams of data analytics.
Factors to consider for your 340B contract pharmacy network
Pharmacy fees
Pharmacy fee structures, and your resulting 340B contract pharmacy revenue, can vary wildly.
TPA fees | TPA compatibility with your 340B contract pharmacies
In addition to pharmacy fees, TPAs often charge for simply attempting to process 340B prescriptions — whether they’re eligible or not. We know of one TPA that charges 30¢ for every attempt.
340B Manufacturer restrictions
Many manufacturer restrictions limit 340B replenishment for certain medications to just one pharmacy per health system. Pick the wrong 340B contract pharmacy for a particularly costly manufacturer-restricted 340B drug that your providers routinely prescribe, and the consequences for your savings and revenue can be catastrophic.
Negotiated pricing for specialty drugs
Fees from specialty pharmacies also vary for 340B prescriptions. Some charge cost-plus percentage, some charge flat rates.
What should you avoid in your 340B pharmacy contracts?
The answer is complicated. And it typically applies on a market-by-market basis. In our experience, here are three primary situations you should avoid:
- Processors who charge on a per-claim basis, coupled with high-volume pharmacies — which will lead to excessive transaction fees for your health system.
- Contract pharmacies with low participation rates in allowing replenishments — picking and choosing which medications you’ve already approved.
- Remotely-located pharmacies offering very few of your patients proximity convenience.
At the same time, hospitals can compromise the potential of their 340B programs by setting Dispensing fees set too low — which lowers local pharmacies’ incentive to partner with you in the program. The time-honored business aphorism applies: In order for your contract pharmacy relationships to reach their full potential, your agreements have to create Win-Win situations for both parties.
Audit requirements
In order to maintain 340B compliance, your health system is required to provide oversight of all contract pharmacies — while maintaining auditable records. You’re also expected to conduct annual audits of your contract pharmacies. Audits which should be completed by an independent auditing firm.
That said, when you authorize VytlOne to manage and/or oversee your contract pharmacy agreements, we’ll give you complete support in maintaining auditable records, and conducting your annual audits.
ADDITIONAL READING
Are your contract pharmacies optimizing your hospital’s 340B savings?
Take full advantage of specialty drug discounts
Specialty drugs, which Medicare defined (in 2019) as any drug costing more than $670 monthly, constituted about 50% of the overall prescription drug market’s expenditures (some $161 billion) in 2020. That’s a 29% increase of total expenditures over 2015. What’s more, according to Acentrus Specialty, 8 out of every 10 new drugs approved by the FDA in 2020 were specialty drugs. All of which makes specialty drugs the fastest-growing, and largest part, of the prescription-drug market.
Specialty pharmacies generate fewer 340B-eligible claims, and higher net savings
According to the estimates of several online sources, the average retail pharmacy prescription in 2020 cost $566 per month — while the average specialty drug prescription cost $6,565. AARP estimated, in a September 2021 article, that —in 2020 — the average annual cost for a single specialty medication used on a chronic basis was $84,442.
340B exposure risk is decreased.
Fewer claims means less exposure to potential audits and compliance claims. What’s more, most specialty pharmacies have dozens, even hundreds, of 340B contract pharmacy relationships; which means that they’re highly experienced, and educated, in maintaining 340B compliance for the covered entities they serve.
ADDITIONAL READING
How do I take advantage of the 340B program for my Specialty Pharmacy?

Implement a robust Meds To Beds program
Benefits of a Meds To Beds Program: Overview
On a purely practical level, a well-managed bedside prescription delivery program can improve your health system’s pharmacy revenue.
On the human level, Meds To Beds is more than a tangible sign of your system’s care of, and for, the individuals & families you treat. It’s your first line of offense in ensuring that your patients follow the prescription protocols you’ve given them — significantly decreasing the likelihood of their readmission while, in the process, improving your patient’s satisfaction ratings.
In general, health systems fail to implement Bedside Prescription Delivery programs because of the costs of staffing and administrations. In our experience, managing dozens of Meds to Beds programs, those costs are more than offset by the revenues generated. In one Mississippi health system alone, VytlOne filled over 18,000 outpatient prescriptions in just 12 months. During that time, the health system’s pharmacy revenues increased 125%, while its readmissions decreased 79%.
How a good Meds To Beds Program works
First, your health system’s retail pharmacy staff must commit to partner with your case management teams, nurses and physicians to implement a cohesive medication treatment plan for your patients who are transitioning back to their lives at home. That commitment means your pharmacy staff must be willing to perform the work necessary to enhance your health system’s current efforts, ensuring that there is never any additional burden placed on your hospital’s providers, nurses and staff.
Next, when prescriptions are delivered bedside to discharging patients, you should be sure to have a pharmacist available to help patients —reviewing both prescription protocols and any issues that could compromise your patients’ willingness (or ability) to maintain compliance with their prescriptions after they leave the hospital.
Once a patients accepts his or her prescriptions, and understands how to maintain compliance, your meds to beds program should pass-off the job of continued patient contact to a readmission risk reduction program.
How Meds To Beds benefit 340B drug programs
Bedside prescription delivery is arguably the most effective method for ensuring that your patients’ prescriptions are captured before they leave your care.
Put another way, your Meds To Beds program should not only support health systems' mission of maximizing patient care, compliance and satisfaction while minimizing readmissions, it should serve as a funnel for directing patients into 340B programs. This role is particularly significant, when you consider the aggressive efforts manufacturers have undertaken to minimize the number of pharmacies that 340B-eligible hospitals can utilize in their 340B programs.
Many manufacturers have launched initiatives to limit their support of eligible entities’ contract pharmacies to one per hospital. They’ve also fought HRSA’s efforts to overturn those limits, through protracted legal battles. It goes without saying, those manufacturers have determined that legal battles are less costly to them than upholding their legal obligation to support 340B drug discounting.
How Meds To Beds benefits your 340B patients
Patients entered into your 340B program “funnel” generally receive superior ongoing professional care and support, after they are discharges. And as we’ve mentioned elsewhere, hospitals with multiple contract pharmacies in their networks offer patients more choices, and convenience, in filling their prescriptions.
Statistical research conclusively demonstrates that two primary factors driving patient non-compliance are lack of education and understanding, and lack of access (both in terms of financial means and proximity) to pharmacies. Which is why many hospitals with 340B programs supplement their Meds To Beds programs by offering home delivery and prescription discounts to financially-challenged patients. Those health systems generally agree that the costs of additional patient support are more than offset by the benefits of superior post-discharge care — not to mention the savings that come with reducing readmissions.
According to a 2020 study published by Frontiers In Public Health, Meds To Beds programs have been shown to significantly reduce 30-day hospital readmissions — particularly among older adult patients.
VytlOne’s Impact© Readmission Reduction Program
In late 2023, VytlOne took all the fundamental components of its Meds To Beds programs, and developed a 30-day readmission reduction program we call Impact®.
Using a clinical pharmacist in collaboration with a health system’s nursing team, the program emphasizes personal, one-on-one patient education and medication-compliance support. The program operates as a separate service from Meds To Beds prescription delivery, but it can easily work in collaboration with MTB. All that’s needed to add Impact® to a Meds To Beds program is an onsite clinical pharmacist and a virtual team of nursing care coordinators.
As we reported in a blog post detailing the program’s initial implementation (at South Carolina’s Conway Medical Center), when our program launched in November, 2023, CMC’s health system had a baseline 47% readmission rate among MVP patients with three or more encounters. After 15 months, our program had enrolled and served 474 participants — and achieved a readmission rate of just 10.1%. Of those patients, past the 30 day mark, 379 patients “graduated” without readmission — and there were only 48 readmits, for an 88.5% graduation rate. Readmissions dropped 77% among patients with 3 or more encounters, and 93% among patients with uncontrolled A1C.
The savings CMC achieved in readmission avoidance costs, as a result of the program, was $1.25 million (based on the $15,200 readmission cost per patient cited above). What’s more, patient satisfaction ratings with the program (142 survey respondents) was 9.77 out of 10 — nearly 50% higher than the national average of 6.6 for health system Hospital Consumer Assessment of Healthcare Providers and Systems Survey (HCAHPS) scores.
To read the full blog post (which includes a video), click the link below:
How To Achieve Readmission Reduction, One Patient At A Time
To read a profile of the program’s Clinical Pharmacist, Click Here.

Understand, and overcome, your TPAs’ limitations
TPAs play a critical role in 340B programs. It’s their job to “match” prescription claims from your contract pharmacies with patient data hospitals provide, and then to determine the eligibility of those claims. Without a match, a prescription cannot be qualified for 340B eligibility and savings.
Your TPAs’ ability to accurately qualify your 340B claims is only as reliable as the information you provide. Their systems simply aren’t configured to monitor and spot mismatches in that data.
340B data mismatches can be extremely trivial.
One of the most common reasons 340B claims are misqualified — particularly with Medicare patients — is inconsistency in Date Of Birth entries. Patient Name mismatches is another common cause of misqualifications. For instance, you may have a patient registered as Bob in your pharmacy system and Robert on your hospital’s system.
That said, the more complex 340B programs are, the higher the likelihood that their automated data submission process will be flawed. Which will naturally lead to missing EHR encounters and missed 340B savings opportunities — quite possibly substantial savings opportunities.
Technology often causes 340B data mismatches
The process of monitoring 340B programs is especially difficult when multiple TPAs are involved. Every TPA’s proprietary software system’s interface is unique. Making matters even more complicated, the reporting structure within TPA portals vary significantly from one to another. We’ve found that health system 340B personnel often spend an inordinate amount of time simply trying to access the information that they need — which leaves them far too little time to proactively take advantage of that information.
How common are TPA 340B misqualifications?
Mismatch rates vary from health system to health system, but we can say this with confidence: If you have a 340B program already in place, it’s probably a lot higher than you think.
One of the health systems VytlOne serves employs three experienced and well-trained full-time professionals — who monitor their system’s 340B claims on a full-time basis. And yet, during the first six weeks VytlOne supported their efforts, we provided matching justification for, and generated $187,000 worth of, 340B savings that they’d overlooked.
WANT OUR RESOURCE GUIDE
IN DOWNLOADABLE PDF?
Chapter 4: Maintaining 340B compliance
How common are 340B health system audits?
Since 2015, HRSA has conducted roughly 200 340B audits annually. On June 17, HRSA reported that it had conducted 163 audits — which would equate to 356 audits for all of 2025.
Manufacturers are legally entitled to audit 340B entities, but since those audits require HRSA approval, they’re extremely rare. Another likely reason for the rarity of those audits is the potential for manufacturers to expose themselves to being audited. HRSA has conducted three audits of drug manufacturers this year, and — in every instance — found that the manufacturers audited were overcharging 340B entities.
Overview: The audit process
Selection for Audit
HRSA conducts both targeted and random audits of covered entities. Targeted audits generally occur when a manufacturer reports suspected diversion or duplicate discounts, the entity has had prior compliance issues, or there are unusual purchasing or prescribing patterns. Random audits are selected from the overall pool of covered entities, and entities typically receive notification letters several weeks in advance.
Audit Notification and Preparation
HRSA will notify the entity of the audit’s scope (which outpatient sites, contract pharmacies, and time period), as well as the audit date(s) and format (on-site or virtual).
HRSA will also make a data request, for which the entity must submit:
- 340B policies and procedures.
- Lists of all 340B-eligible sites and contract pharmacies.
- Drug purchase and dispensing data.
- Patient encounter documentation.
The entity is then expected to conduct internal reviews and confirm its data accuracy before the audit begins.
Audit Fieldwork
Whether HRSA conducts its audit on-site or virtually, HRSA’s auditors will:
- Review sampled drug transactions to ensure they meet 340B eligibility.
- Determine if any 340B drugs were diverted to ineligible patients or sites.
- Check for any duplicate discounts (IE: That Medicaid claims were properly flagged or not).
- Examine the entity’s policies, systems, and oversight processes.
- Interview staff involved in pharmacy, compliance, and data management.
Post-Audit Process
After fieldwork, HRSA will issue a Draft Report, after which the covered entity will have the opportunity to respond to preliminary findings and provide clarifying documentation or corrective evidence.
Once HRSA finalizes its findings, a Final Audit Report is published on the HRSA website.
Possible outcomes include:
- No findings (fully compliant).
- Findings of non-compliance, typically involving:
- Diversion (340B drugs dispensed to ineligible patients or sites).
- Duplicate discounts (Medicaid rebate plus 340B discount).
- Database inaccuracies (IE: Outdated contract pharmacy listings).
Corrective Action and Repayment
If HRSA confirms non-compliance, the entity must submit a Corrective Action Plan (CAP) detailing how it will fix the issue(s), and how it will prevent recurrence. HRSA requires repayment to affected manufacturers for any ineligible discounts received. Finally, HRSA may re-audit to verify sustained compliance.
Additional factors impacting 340B compliance in 2025
340B data transparency requirements
New scrutiny from lawmakers and regulatory agencies is prompting calls for better 340B program recording, tracking and reporting. Which is why the need for customized, analytics-driven technology has never been more critical to ensuring 340B compliance. At the same time, the need for proven experts to manage your 340B program has never been greater.
Learn More:
Empower Your Health System’s 340B Program With Analytics
Specialized Software Can Only Do So Much For 340B Programs
A 340B Program Compliance Checklist
340B is complicated. That’s why so many covered entities have full-time employees monitoring their 340B programs. At the same time, for the clients whose 340B programs we manage, VytlOne performs all the duties of a dedicated full-time staff — and more.
Below is a condensed checklist of safeguards we implement to help ensure the success, and full compliance, of every 340B program we manage and support. Safeguards you can use for your own program:
- Develop written policies & procedures that detail all of your 340B-related decisions.
- Make sure your 340B policies are compatible with your hospital’s existing policies and procedures.
- Double-check your provider files — as well as your National Drug Code crosswalks and the location maps for all of the contract pharmacies in your network — for accuracy.
- Utilize customized, analytics-driven software that’s been specifically developed to ensure that your 340B information is always up-to-date.
- Maintain a constantly-updated database of strategies and tactics for dealing with 340B ESP and other manufacturer restrictions (See Chapter 5 below for a complete overview).
- Support your providers, by giving them complete information on 340B program regulations, and how those regulations work with your hospital’s existing policies & procedures.
- Conduct regular inventory-management and tracking-procedure checks, to ensure that you’re always in compliance.
- Establish a Governance Committee to meet regularly and review your health system’s 340B program.
- Conduct regularly-scheduled internal audits of your health system’s 340B program.
This final point is worth repeating: Routine self-audits are critical to ensuring your program’s compliance.
Carve-in or Carve-out?
When you register your health system for the 340B program, you’ll be asked to choose whether you’ll Carve-In or Carve-Out Medicaid fee-for-service (FFS). This decision will apply to all of your Medicaid FFS patients. Choosing Carve-In means that you’ll be using 340B-priced medications with your Medicaid FFS patients. Choosing Carve-Out means you will not use 340B-priced medications with your Medicaid FFS patients.

Avoid 340B Double-Dipping
The 340B program does not allow you to take advantage of 340B discounts and Medicaid drug rebates for the same drugs. That’s the practice known as Double Dipping, and as a covered entity, you need to maintain compliance mechanisms that prevent duplicate discounts.
Preventing 340B double-dipping begins at enrollment
If you decide to Carve-In Medicaid fee-for-service, you’ll be required to list each Medicaid state where plan to bill, as well as the corresponding billing number(s) you’ll list on your bills to those states. It follows, then, that you shouldn’t list any Medicaid states where you plan to carve-out.
Common 340B Errors to avoid in your program
Poor tracking. You must be able to prove that every drug purchased on your 340B account is administered to an eligible patient from an eligible point of service.
Lack of contract pharmacy oversight. As a covered entity, you’re ultimately responsible for monitoring your contract pharmacies and ensuring that they maintain compliance with all 340B program requirements. If you identify any diversions or duplicate discounts, it’s your responsibility to notify the Office of Population Affairs (OPA) of the violation — and offer a remedy.
Failing to register all of your Child sites. Even if you have child site inside your hospital, or another registered primary facility, you should register it. That way, if you ever need to move that child site, you won't have to go through the registration process — and that typically takes six to nine months, sometimes an entire year. And during that time, you will not be legally entitled to 340B savings.
Want Our 2025 Compliance Checklist In Downloadable PDF?
CHAPTER 5: 340B ESP & manufacturer restrictions, and how to overcome them
What is 340B ESP?
According to its website, “340B ESP allows 340B covered entities and pharmaceutical manufacturers to work collaboratively to resolve duplicate discounts.” In truth, the “service” is a brazen, unlawful ploy by drug manufacturers to evade the prescription-replenishment discounts they are legally required to offer eligible entities — by placing extraordinary reporting burdens on hospitals submitting claims for 340B savings.
The real reasons behind 340B ESP?
We believe the key factor that led to 340B ESP is the extensive range of commercial rebates the manufacturers themselves have voluntarily extended to PBMs — rebates which, in total, far exceed the combined discounts extended to 340B-eligible hospitals and health systems. In short, it's a situation of their own making.
340B ESP’s additional “hidden motives”
The 1400-member 340B advocacy group 340B Health notes that “claims data and other information submitted through the 340B ESP platform could be used by the Berkeley Research Group (BRG), the entity behind Second Sight Solutions [which owns 340B ESP], for research and analytics. BRG has published a number of negative reports on 340B in the past that have been funded by [the trade association formerly known as the Pharmaceutical Manufacturers Association].”
In short, there is a very real possibility that BRG could be using 340B pricing claims data submitted to 340B ESP to undermine the very entities it purports to be “serving.”
340B ESP’s “Terms Of Use” are absurd.
In unedited form, 340B ESP’s Terms Of Use runs 5798 words in length. Based on the average adult’s speed in reading technical documents (62.5 words per minute), that means 340B ESP’s terms of use alone will take the average reader nearly 93 minutes to complete. That estimate, of course, constitutes a fraction of the time it would take most health systems' 340B-reporting employees to read and fully comprehend the terms.
Excerpts from the 340B ESP Terms Of Use
###
The Covered Entity Platform is subject to modification (including addition, alteration, or deletion) by Second Sight in its sole discretion.
###
Upon termination…Second Sight shall have no obligation to return to you any data stored on Second Sight's systems.
###
You expressly acknowledge and agree that the Participating Pharmaceutical Manufacturers are third party beneficiaries of these Terms and have the full rights to enforce these Terms as if any one of them was a signatory hereto.
###
Second Sight may revise these Terms from time to time by posting such revised Terms on this website, or otherwise notifying you in advance of making effective such revisions to the Terms. Such revised Terms shall be effective to you upon the effective date provided in the posting or other notice, unless otherwise explicitly stated by Second Sight. It is your responsibility to be aware of any such revised terms by checking and reading these Terms from time to time and your notices.
Excerpt from 340B ESP’s Limitations Of Liability section
THE LIMITATIONS OF LIABILITY SHALL NOT APPLY TO SECOND SIGHT'S GROSS NEGLIGENCE OR WILLFUL MISCONDUCT. SECOND SIGHT'S AGGREGATE LIABILITY FOR DIRECT DAMAGES UNDER THIS AGREEMENT WILL NOT EXCEED ONE HUNDRED DOLLARS ($100).
The reporting burdens 340B ESP place on covered entities
Under the requirements set down by Drug Manufacturers, 340B-eligible entities must report, twice monthly through the 340B ESP platform, their covered prescriptions from every TPA with whom they work.
Extracting covered prescription data from some TPAs is impossible, given the lack of available 340B pricing in the 340B wholesaler account. Moreover, it’s pointless to assume that covered entities and their contract pharmacies will regain access to their 340B discounts — since some manufacturers have placed 45-day time-frame restrictions from the dispensing of the prescription to replenishment. Why? They know that covered entities won’t be able to meet this requirement.
How effective has 340B ESP been in enabling drug manufacturers to evade their legal obligations? In the first year of its relationship with 340B ESP, Merck alone saved $2 billion. Worse still, at last count, 18 manufacturers are now requiring eligible health systems to report to 340B ESP.
How we help eligible entities deal with 340B ESP
If you choose to report claims data to 340B ESP, we’ll report on your behalf. Then we’ll track 340B price reinstatement — by manufacturer, and by contract pharmacy. We’ll also verify 340B price availability for each manufacturer, in each wholesaler account, for each of your contract pharmacies. Once verified pricing has been restored along the entire chain, we’ll work with your TPAs to ”turn-on” replenishment — and ensure they replenish appropriately.
Reporting to 340B ESP
- VytlOne tracks, on a per-manufacturer / per-pharmacy basis, 340B price eligibility according to what 340B ESP claims it is.
- We then verify in each 340B account — by Consumer Pricing and by manufacturer — if what 340B ESP claims is accurate.
- Once we’ve verified each data point, we’ll notify your TPAs of newly restored pricing — then ensure that they request new price files from wholesalers.
- Once your TPAs have 340B prices, we’ll order the 340B eligible drugs.
There are many places where communication-failure can and does occur — which is why we communicate with manufacturers, 340B ESP and wholesalers on your behalf. After that, we fight for reinstatement of the prices to which you’re entitled under the 340B statute.
Six Common 340B ESP Reporting Errors
1. Uploading Excessive 340B Data
Never upload more data than is absolutely necessary, and required, by 340B ESP. We submit the NDCs only from the manufacturers imposing restrictions on 340B pricing contingent on data reporting.
2. Trusting 340B ESP to Restore Prices On Its Promised Scheduling
Don’t ever assume that 340B prices are restored in your contract pharmacies’ 340B wholesaler accounts by the 10-day post-submission mark (the time frame 340B ESP says to allow).
3. Trusting 340B ESP Price Restoration, Period
If any manufacturer working with 340B ESP decides, unilaterally, that the purchases made for any of your contract pharmacies are more than the dispenses, they’ll refuse to pay the wholesaler’s chargeback. Which will result in a credit-rebill — which results in you, the covered entity, paying WAC — which is a much higher price.
4. Assuming submitted eligible dispenses result in 340B price access
Eligible 340B dispenses often do not occur in full-package-size increments. It may take months, and multiple claims, to equal a full reorderable package size — but some manufacturers won’t reimburse 340B purchases past 45 or 60 days from dispense. Which means covered entities will likely never be able to get many of the 340B prices they are entitled to.
5. Counting-On 340B ESP-Compatibility In Your TPAs’ Reports
When you submit your own reporting to 340B ESP, you can’t simply pull reports, verbatim, from your TPAs and upload them. Your uploads must be submitted in a highly-specified format, and every upload is fraught with potential pitfalls that can cause failures.
6. Counting-On Support From 340B ESP
In our experience, nobody working with 340B ESP — or the manufacturers — will help you when you don’t receive the 340B prices to which you’re entitled, even if months have passed since your first data submission.
The good news about 340B ESP, for covered entities
Despite 340B ESP and manufacturer restrictions, VytlOne continues to produce results for health systems. Since late 2019, we've supported the 340B programs of 33 health systems and 38 health centers. Altogether, we’ve generated nearly $1 billion in pharmacy-related savings for our clients.
VytlOne is here to help, if you have questions.
There are so many ways to optimize your 340B savings and revenue, while overcoming 340B ESP and manufacturer restrictions. For more information, contact Howard Hall. C: 214.808.2700 | howard.hall@VytlOne.com

Manufacturers Accelerate 340B Drug Pricing Restrictions
There’s an old saying that it’s better to be rich and guilty than poor and innocent. It’s a sad truth that accurately reflects the current state of 340B manufacturer restrictions, particularly in the wake of the January 30, 2023 decision by the U.S. Court of Appeals for the Third Circuit — which was largely in favor of three drug companies that have imposed harmful limits on safety-net hospitals’ access to 340B drug pricing program discounts.
Novartis introduced a new tactic to evade its 340B obligations.
Novartis was the first drug manufacturer to limit 340B-eligible contract pharmacies to those located within 40 miles of the covered entity will have pricing added. On the surface, this doesn't seem particularly problematic. After all, most, if not all, of a typical 340B-eligible health system’s retail contract pharmacies — from chains to local independents — will still get 340B pricing. The problem with the 40-mile radius, and Novartis knows this, has to do with covered entities’ specialty pharmacy networks.
The number of specialty pharmacies across the country is significantly lower than the number of retail pharmacies — and a significant percentage of those pharmacies serving 340B-eligible entities are located outside that 40-mile radius.
On top of that, there’s the difficulty of 1) getting PBMs to allow pharmacies to dispense for their patients — other than the pharmacies health systems own — and 2) getting manufacturers to allow purchase of their specialty meds.
Johnson & Johnson’s 340B restrictions are even worse.
On February 15, 2023, one of the clients we serve forwarded us a 10-page, 3914-word letter they’d received from Johnson & Johnson. After they’d spent who-knows-how-many-hours poring over the contents, their email included one genuinely troubled question: “Does this mean what we think it means?”
The key restriction to which they were referring (which Johnson & Johnson announced would go into effect starting March 7, 2023) was as follows:
If a non-grantee Covered Entity does not have an in-house pharmacy, such Covered Entity may designate a single contract pharmacy location registered on the HRSA OPAIS database for delivery of 340B-priced covered outpatient drugs listed on Attachment A if (I) the Covered Entity provides limited claims data with respect to that contract pharmacy location and (ii) that single contract pharmacy location is within 40 miles of the Covered Entity parent site.
In plain English, Johnson & Johnson is telling 340B covered entities, that — starting March 7 — they can designate only one pharmacy as a contract pharmacy in their networks, AND that the pharmacy has to be located within 40 miles of the health systems’ campuses.
Consider the implications for 340B-eligible patients who lack easy access to transportation: For all practical purposes it means that, unless that single contract pharmacy offers prescription-shipping services, they’re either NOT getting their medication — or they’ll be incurring significant personal costs to fill their prescriptions.
Novartis and J&J’s 340B restrictions violate a core patient right: Choice.
One of the most critical benefits our vast pharmacy industry offers is patient choice. By law, patients have the right to choose where they get their medications. Covered entities don’t dictate which pharmacies their patients use. But when restrictions limit 340B pricing to one contract pharmacy (much less zero pharmacies), they’re robbing patients of their legal right to choose.
Taking their cue from J&J, three more manufacturers — AbbVie, Amgen and GSK — promptly imposed 40-mile restrictions on 340B-eligible claims for their drugs. Then, on April 3rd, Novartis implemented its own “single pharmacy within 40 miles” policy.

The impact of 340B ESP and other manufacturer restrictions
Making the rich richer at the expense of the poorest and most vulnerable.
For 340B covered entities operating without the sophisticated processes and advanced analytical software developed by ProxsysRx, the impact of manufacturer restrictions has been devastating. 340B revenues for numerous covered entities has plummeted. Many of those Disproportionate Share Hospitals rely on 340B revenue to help fund their Uncompensated Care and Community Outreach efforts. And when it comes to uncompensated care, the term Disproportionate Share couldn’t be more accurate. In 2020, the average 340B DSH hospital provided $38 million in uncompensated care — while the average non-340B hospital provided just over $14 million (Source: 340B Health).
Dealing daily with 340B ESP and other manufacturer restrictions
For VytlOne's 340B team, those restrictions have meant an exponential increase in the time involved to ensure that the health systems we serve get the 340B savings to which they’re legally entitled. One VytlOne 340B Program Specialist estimates that he spends the first two to three hours of every day on the job dealing with manufacturer restrictions — and that’s before he’s submitted the first 340B claim for one of the three covered entity accounts he manages.
Manufacturers currently imposing unlawful 340B program price restrictions
As of April 10, 2023, there were 21 manufacturers imposing restrictions — either through 340B ESP, or independent of the website:
- AbbVie
- Amgen
- AstraZeneca
- Bausch
- Bayer
- Biogen
- Boehringer Ingelheim
- Bristol Myers Squibb*
- Eli Lilly
- EMD Serono
- Exelixis
- Gilead
- GSK
- Johnson & Johnson
- Merck
- Novartis
- Novo Nordisk
- Pfizer
- Sanofi
- UCB
- United
Of the 21, nine currently promise to uphold one of the standards established by the 340B program requirements — enabling covered entities to designate and supply claims for an unlimited number of contract pharmacies. That means 12 (or 57%) of those manufacturers are in open violation of the intent of the 340B program — which was created to enable covered entities to use multiple contract pharmacies.
How VytlOne Maintains A Constantly Updated List Of 340B Covered Drugs
Describing just one aspect of his own experience with manufacturer restrictions, one VytlOne 340B Program Specialist notes, “Because they're so ambiguous, and changing so quickly, the restrictions force our team to review all of the restricted NDCs on a daily basis. Every pharmacy we serve has to be cognizant of all 1628 restricted NDCs when submitting prescriptions for 340B savings. And when a covered entity has multiple contract pharmacies, there's a multiplier in tracking NDC's and prescriptions.
“Each one of our team members is literally monitoring thousands of prescriptions on a daily basis. Which is one reason our team continues to grow. And why our clients have benefited so greatly from the 340B PRO software we developed, which has enabled us to grow and scale. Because you don't just have a single question needing answers on every prescription. It's not just about the NDC's. There are layers and layers of problem-solving involved.”
ADDITIONAL READING
Manufacturers Accelerate Pace And Severity Of 340B Drug Pricing Restrictions

Why specialized software is essential for successful 340B programs
Without specialized software solutions, the average 340B-eligible health system would likely need a dozen (or more) full-time employees, just to monitor their prescriptions to maximize savings and revenue. VytlOne rolled-out the first version of 340B Pro in 2021, and we are constantly updating and adjusting it to deal with the ever-evolving challenges manufacturers introduce in their 340B pricing restrictions.
340B programs need TPA support, but TPAs are far from perfect
TPAs’ systems are not especially adept at monitoring and spotting provider / entity data mismatches — which are common occurrences in 340B programs. Nor do their fees generally incentivize them to improve their performance. That’s why helping health systems minimize data mismatches at the source is so critical to maximizing 340B drug pricing program savings for a covered entity — and why meeting that challenge is a core component of our 340B software and service package.
The critical role humans play in the 340B software equation
Over the years, VytlOne's software has identified untold millions of dollars’ worth of 340B-eligible prescriptions missed by the TPAs working with hospitals we serve — as well as with their contract pharmacy networks. However, software solutions alone can’t reliably requalify prescriptions for 340B drug pricing program savings — for the simple reason that there has to be a reason each prescription is requalified. And that reason has to be defensible, if it’s challenged in audit.
All of that requires 340B program management experience and judgment on a prescription-by-prescription basis, and as anyone familiar with technology can tell you, Artificial Intelligence still has a long way to go in solving problems that require nuance and insight.
What’s more, when a prescription is coded incorrectly by a provider — which happens regularly in even the best-managed 340B programs — it creates what amounts to a Domino Effect of incorrect coding throughout the step-by-step process of submitting that prescription for reimbursement. Without the intervention of an experienced 340B manager, TPA software can actually make the situation even worse.

How VytlOne overcomes manufacturer restrictions on 340B pricing.
As much as we’d love to report that we’ve discovered the proverbial magic bullet for piercing manufacturer barriers to optimizing 340B cost savings and revenue, we can’t. Our process starts with an in-depth assessment of a health system’s current 340B-program status (assuming the health system has an active 340B program). Once we’ve conducted that analysis, we work with the health system’s 340B professionals to develop strategies for improvement in every area of its program. VytlOne's 340B support team then implements software-supported processes for auditing missed opportunities.
For most of the hospitals we serve, VytlOne's team also provides hands-on support in managing their 340B programs.
The good news is, our process is producing results. And while those results vary from system to system, one of the small rural hospitals we serve has seen a monthly net savings increase of more than 900% over their historical averages since manufacturer restrictions were implemented.
Below are the seven key elements of our process.
1. Establish communications between health system providers and their outpatient pharmacies.
With manufacturer restrictions, it’s more important than ever that health systems have onsite pharmacies partnering with them to capture as many 340B-eligible prescriptions as possible — in part, to ensure that savings stay within the system, thereby enabling them to pass-along those savings to patients.
2. Upload only the 340B Data required, and NO MORE.
As with every aspect of our program, we learned this lesson through experience: When working in the 340B ESP platform, you should never upload any data that isn’t absolutely required by the platform. We submit the NDCs only from manufacturers that impose 340B pricing restrictions that are contingent on data reporting.
3. Do NOT trust 340B ESP to restore prices on its promised scheduling.
340B ESP says health systems should expect a period of 10 days, post-submission, for 340B prices to be restored in their contract pharmacies’ 340B wholesaler accounts. In reality, that rarely ever happens within 10 days — if at all. Which is why VytlOne has implemented a system for checking all NDCs, in all of our health systems contract pharmacies’ 340B accounts, before instructing their TPAs to restart processing on any restricted NDCs.
4. Do NOT trust 340B ESP price restoration, period.
Health systems cannot assume that any 340B price restorations they have will actually be honored. Manufacturers working with 340B ESP routinely, and unilaterally, decide that the purchases made for arbitrarily-selected contract pharmacies are more than the dispenses.
5. Don’t assume that submitted eligible dispenses result in 340B price access.
Some manufacturers now require you to submit 340B purchase data reports within 45 or 60 days from dispense — or they disallow those submissions. Although VytlOne mines clients’ 340B-submission records for eligible prescriptions missed by their TPAs, the time frame is tight with these arbitrary, fraudulent manufacturer requirements — and thus far, we’ve yet to develop a workaround for dealing with them.
6. Don’t assume that 340B ESP will be compatible with your TPAs’ reports.
If you’re thinking you can simply pull reports from your TPAs and upload them, when submitting your own reporting to 340B ESP, think again. Most TPAs’ reports require significant modifications first. Your own uploads have to be submitted in 340B ESP’s exactingly-specified format, and every upload has the potential for reporting errors that can cause failures.
7. Don’t bother asking 340B ESP for help.
Nobody working with 340B ESP — or the manufacturers — has ever helped our team when our clients didn’t receive the 340B prices to which they’re entitled, even when months have passed since we made data submission.
VytlOne is here to help, if you have questions.
There are so many ways to optimize your 340B savings and revenue, while overcoming 340B ESP and manufacturer restrictions. For more information, contact Howard Hall. C: 214.808.2700 | howard.hall@vytlone.com
WANT OUR RESOURCE GUIDE
IN DOWNLOADABLE PDF?
Chapter 6: Using specialty pharmacy to optimize 340B revenue and patient outcomes
Why a 340B specialty pharmacy?
The ultimate Win-Win scenario for any health system is increasing the quality of patient care, and getting paid to do it.
Chronic illnesses have become increasingly common in the United States. According to a report by The American Hospital Association, the number of Americans with chronic medical conditions will grow by a projected 14 million people between 2020 and 2030. According to some online reports, nearly 80% of new drug introductions are now specialty medications.
Moreover, for 340B-eligible hospitals dealing with increasingly squeezed bottom lines, an in-house specialty pharmacy offers enormous savings and revenue potential. Some covered entities generate as much as 600% in specialty pharmacy revenue from 340B drugs as they do in traditional retail / outpatient pharmacy 340B revenue.
Better patient outcomes. Better health system incomes.
In short, the reason 340B hospitals should build onsite specialty pharmacies is the significantly increased potential for generating 340B savings — and for passing-along those savings to patients in need. Today, hospitals and other 340B covered entities can acquire many specialty drugs for as little as 1¢ — which happens when a drug has hit its 100% Medicaid rebate cap.
In 2016, Humira, the top-selling drug in the U.S., hit the rebate cap. Since that time, 340B hospitals have been able to buy Humira, and many other specialty drugs — including Epclusa, Harvoni, Imbruvica, Iressa, Gilenya, Revlimid and Stelara — at significantly-reduced prices.
Nearly 90% of all large, for-profit hospitals are already operating their own specialty pharmacies. Ultimately, it stands to reason, every 340B health system looking to increase pharmacy revenue will need to consider building their own.
Streamlining 340B patient care
Onsite specialty pharmacies in 340B hospitals offer a seamless approach to caring for the “sickest of the sick” patients they serve. With their expertise, pharmacists at your onsite specialty pharmacy can collaborate closely with your health system’s providers, effectively managing complex medication regimens — while minimizing the risk of medication errors.
Enhancing 340B-patient medication adherence
Medication non-adherence is the number one cause of unnecessary patient readmissions. Onsite pharmacies can play a pivotal role in improving medication adherence among patients likeliest to burden hospitals with costly, compliance-related readmissions.
Working in tandem with its retail pharmacy, a hospital’s specialty pharmacy can create efficient solutions to help manage prescription loads. Onsite specialty pharmacists can engage patients in one-on-one counseling, providing them with essential information about their medications' purposes, potential side effects, and proper administration.
Expanding 340B-patient access to specialty medications
The top two reasons for patient noncompliance with medication protocols are 1) the prohibitive cost of their prescriptions, and 2) the limited availability of those prescriptions. Onsite specialty pharmacies in 340B hospitals can overcome those problems by procuring 340B specialty drugs at discounted prices.
340B specialty-medication cost savings
With your own onsite specialty pharmacy, your hospital can capture a greater percentage of the 340B revenue that would otherwise go to outside pharmacies — supporting your financial stability, while enabling you to expand healthcare services and make infrastructure improvements in serving your community.
Improving overall patient satisfaction
Patient satisfaction is an increasingly essential aspect of the Quality Ratings that impact many 340B health systems’ reimbursement rates.
Onsite 340B specialty pharmacies can contribute to higher satisfaction levels in several ways:
- Reducing patient wait times
- Offering patients greater access to tailored medication services.
- Improving patients’ confidence in their treatment plans.
- Increasing overall trust in the healthcare system.
- Ensuring greater levels of medication compliance.
Facilitating clinical research and innovation
Onsite specialty pharmacies can serve as valuable resources for 340B hospitals conducting clinical research — promoting medical innovation and, ultimately, benefiting patient care for everyone.
Leveraging 340B Data Analytics
The integration of onsite specialty pharmacies within 340B hospitals enables the collection and analysis of comprehensive patient data. With enhanced data-driven insights, 340B hospitals can continually improve their patient care protocols and optimize treatment outcomes.
Overcoming 340B ESP And Drug Manufacturer Restrictions
The majority of 340B-eligible medications under access-restrictions are the most expensive and profitable drugs — which often means specialty drugs. This includes the aforementioned 40-mile-radius restriction and the Single Contract Pharmacy restriction.
Fortunately, there is a workaround for 340B hospitals forced to select a single pharmacy for certain manufacturers’ 340B pricing — and it’s legal in many states. Hospitals can operate specialty pharmacies alongside their retail pharmacies IF the two operations are in separate spaces (with separate Pharmacists-In-Charge), and there is no procedural, functional or personnel overlap between the two.
The not-so-good news for 340B hospitals is: Opening a specialty pharmacy is extremely challenging — particularly given the effort required just to get access to purchase specialty meds, and then to get “In Network” with PBMs. Payers and manufacturers control the players in Specialty, so newcomers need significant support and guidance navigating the process. That doesn’t even account for how hard it is accrediting and running a Specialty Pharmacy.
Reasons why you should NOT own a specialty pharmacy.
The not-so-good news for 340B hospitals is: Opening a specialty pharmacy is extremely challenging — particularly given the effort required just to get access to purchase specialty meds, and then to get “In Network” with PBMs. Payers and manufacturers control the players in Specialty, so newcomers need significant support and guidance navigating the process. That doesn’t even account for how hard it is accrediting and running a Specialty Pharmacy.
Here is a fairly inclusive list of reasons why owning a specialty pharmacy is tough:
Owning a 340B specialty pharmacy is expensive.
- It’s expensive to build.
- It’s expensive to accredit with URAC and ACHC.
- It’s expensive to staff.
- It’s expensive to stock.
- It’s expensive to operate and maintain.
- It’s expensive to grow.
Owning a 340B specialty pharmacy is complicated.
- It’s complicated and time-consuming getting accredited.
- It’s complicated and time-consuming getting in-network with payers.
- It requires a lot of internal committee and administrative oversight, and that requires dedicated administrative resources and interdepartmental coordination.
- It’s significantly more “regulated” than a retail pharmacy. Specialty pharmacies must comply with complex and frequently evolving requirements from HRSA, FDA, payers and accrediting bodies.
- It requires specialized technology and processes for everything from prior authorization and inventory management to outcomes tracking.
- It requires a significantly higher level of ongoing data collection and reporting.
- It’s subject to far more manufacturer restrictions, on average, than a retail pharmacy.
So, should you own a specialty pharmacy, and if so, why?
The simple answer is: It’s worth it. Experience has taught us that all of the additional costs and complications of owning an onsite 340B specialty pharmacy are more than offset by the benefits it offers to the patients in greatest need.
And while it’s true that offsite 340B contract specialty pharmacies costs you less, but the returns — clinical and financial — are much lower. After all, independent specialty pharmacies are, by necessity, more focused on supporting their business objectives than your own specialty pharmacy would be.
How VytlOne makes it easier for 340B hospitals
We guide the health systems we serve through the process steps that they’re required to participate in. Fortunately, those steps tend to be the least burdensome in the process. We handle the rest of the process — painstakingly documenting everything we do, and reporting back to the health systems at every critical step.
By Q2 2025, we were in the development process for specialty pharmacies with seven health systems and several FQHCs. In 2024, we helped build, fund and open a specialty pharmacy for a large regional 340B hospital located in the Southeast; within six months of its launch, the pharmacy began generating a monthly income of $1 million net. More important is the fact that the pharmacy began positively impacting the quality and scope of the health system’s patient care months in advance of its official opening date, and that impact has increased significantly since then.
When VytlOne supports you in building and owning a specialty pharmacy, we’ll get you in-network with payers long before the physical space opens — which will enable you to generate additional 340B revenue to pay for your investment during the process. We can even help you secure a contract to dispense what’s known as “soft” specialty drugs — which you can legally prescribe through your retail pharmacy.
Ensuring your specialty pharmacy’s success
Internal operations are only part of the formula for a specialty pharmacy’s success. Which is why we seek inclusion from all PBMs in a health system’s area. We go in-network, securing cooperation and approval from all the major local insurers, for the PBMs that their patients are covered by. What’s more, we seek access from the drug manufacturers for what they’re prescribing — even the most restrictive manufacturers.
How quickly can an onsite 340B specialty pharmacy pay for itself?
With efficient workflow processes and a fully-leveraged contract pharmacy network, and a large enough patient base needing specialty pharmacy medication, your investment can pay for itself within a few months. That said, specialty pharmacies for larger 340B hospitals tend to pay for themselves more quickly, for the simple reason that they generally have more opportunities for specialty pharmacy prescriptions and savings.

Starting A 340B Specialty Pharmacy: What Does The Process Look Like?
Specialty pharmacies require costly accreditation, both financially and in terms of the time investment. You must contract with payers. Securing each contract takes considerable time and effort. You must provide a tremendous amount of data and analytics to PBMs and manufacturers, to prove that you can provide the level of quality patient care expected of Specialty Pharmacies.
Use your hospital’s retail pharmacy to build a specialty pharmacy
A well-run retail pharmacy can generate significant revenue and profits for your health system. Consider setting-aside a percentage of your 340B retail-prescription savings. By earmarking them for funding the project, you can gradually build-out your onsite specialty pharmacy capabilities — while analyzing your clinics and workflows — without drawing large capital expenditures from your budget.
VytlOne serves 340B hospitals as a retail pharmacy partner
When VytlOne builds-and-owns or manages retail pharmacies for health systems, we only pay ourselves from the revenue and savings we generate on their behalf. We take-on all the risk, so they are never exposed to the potential for loss.
ADDITIONAL READING
Best Practices For A 340B Hospital Looking To Build An Onsite Specialty Pharmacy
Specialty Pharmacy Best Practices For 340B Hospitals
Meeting specialty pharmacy accreditation standards & policies
As you start building a specialty pharmacy, you can take steps towards accreditation — but you have to make sure that you have the policies, standards and protocols in place to ensure that your specialty pharmacy meets those accreditation standards.
You can actually start filling prescriptions on Day One, but it takes work to find the prescriptions you can fill immediately. Accreditation can take 6 months to a year, depending on the health system and the process of integrating a specialty pharmacy into its resources.
You have to have reporting in place when you begin filling prescriptions. And while you’re filling those prescriptions without accreditation, you're getting in the networks with your PBMs. And then, as you get your pharmacy and process stood up — and its procedures and policies in place — you're able to become accredited.
Specialty pharmacy accreditation metrics
When you become accredited, you have to keep certain metrics for patient phone calls. That means there must be someone in the pharmacy every hour it’s open. Someone who can answer phone calls promptly, so your patients have easy access to a pharmacy professional, who can answer their questions — and make sure they're getting the appropriate care. For accreditation, this confirms that you're a qualified specialty pharmacy, and that you're taking care of your patients in the possible best way.
Specialty pharmacy service-data reporting
There are patient monitoring and clinical assessments that have to be tracked and measured. Every specialty pharmacy patient should be monitored by a clinic pharmacist.
Clinical assessment for specialty pharmacy patients
In initial assessments, specialty pharmacists should ask patients what other medications they’re on, and what side effects they’ve experienced. Specialty pharmacy pharmacists should also work hand-in-hand with patients’ providers, to make sure that medication regimens are appropriate, up to date, and the most accurate regimens for patients and their disease states.
Continuous monitoring & reporting
In addition to ongoing monitoring, most patients should be monitored yearly by pharmacists — to review any side effects they may be having, or any other issues they have taking their medication.
Pharmacists should ask patients if they’ve skipped any medications, and if it’s affected their disease state. Moreover, all of that data should be reported back to the accrediting bodies.
Ensuring patient satisfaction with their specialty pharmacy’s support
Patient satisfaction surveys, conducted by independent third parties, are required — to ensure that you're upholding high standards.
To ensure that you're meeting or exceeding those standards, you should carefully review your specialty pharmacy’s processes. You should also make sure your providers know what it takes to ensure that patients know you care about their outcomes, and that they have the access to the appropriate medication.
Specialty pharmacy shipping & packaging protocols
Most specialty medications are delivered to patients at home. A lot of them require refrigeration, and some have to be frozen. Some need to stay at room temperature, and can't get too hot or too cold.
All of which is why it’s so important that your specialty pharmacy follows shipping and packaging protocols required by the accrediting bodies. You need a Cold Chain Vendor for shipping and packaging medications at appropriate temperatures. You also need processes and policies in to test vendors’ capabilities.
Integrating your specialty pharmacy’s technology with your health system’s technology
VytlOne has its own technology platform in place that pulls all the data, so we can create the necessary outlooks and outputs from our analytical tools. Data we then report back, not only to the accrediting bodies, but also to the payers — the PBMs. That way, when we're getting a specialty pharmacy in-network for a patient’s PBM, we can bill for the patient’s care.
That said, your health system should invest in similar software capabilities for your specialty pharmacy.
Integrating Specialty Pharmacy With 340B
VytlOne's unique approach to specialty pharmacy provides health systems with a financial “glide path” to help fund their specialty pharmacies. One that starts with optimizing their 340B network. We’ve proven that VytlOne can help health systems improve revenues — often by millions of dollars annually — while their specialty pharmacies are being built. More importantly, we do it while helping hospitals improve the quality of patient care.
There are so many ways to optimize a 340B program, while making it more compliant. And it’s changing all the time, so we’re always looking for new ways to ensure that we’re capturing everything coming out a health system.
Avoiding negative specialty pharmacy 340B reimbursements
What causes negative reimbursement? Several factors, including:
- #1 Overlooking 340B dispense status
- Purchasing drugs at WAC instead of on a 340B account
- Receiving 340B specialty pharmacy drugs without PBM access
Overcoming 340B PBM / payor hurdles
Many PBMs will not pay for prescriptions right out of the gate, so there are a lot of hurdles you have to jump with payors to get drugs covered. Even after 340B specialty drugs are covered, copays can be very high — sometimes thousands of dollars. Most patients can't afford copays that high, so you need to know how to get copay assistance. There are a number manufacturer programs, and other assistance programs — including charity care. Learn to use all those options, to make sure your patients can get their prescriptions promptly.
Performing prior authorizations for specialty drugs
Another benefit of having a pharmacist embedded in the clinic where your patients are is: They’re able to look for financial assistance, and perform those prior authorizations — making sure that prescriptions are going to be paid for, and that patients can afford them.
The 340B Retail / Specialty Pharmacy Relationship
Meeting all of a patient’s medication needs
Very often, patients have prescriptions from both a hospital’s retail pharmacy and its specialty pharmacy. Make sure each pharmacy team always knows what the other is doing, as far as providing for those patients — even to the point where patients can routinely call your retail pharmacy with questions, and get answers about their specialty drugs.
Of course, when it comes to anything clinical about patient monitoring, or anything that has to do with high-complexity meds, patients should be connected with clinical pharmacists familiar with their disease states.
You should also ensure that specialty-medication patients speak to your clinical pharmacists before each refill, to answer questions or concerns — and check for medication effectiveness and side effects.
Why VytlOne For Your 340B Hospital’s Specialty Pharmacy?
Helping fund your 340B specialty pharmacy
VytlOne helps health systems create a financial glide path to build their specialty pharmacies. A path that ensures the burden of financing their specialty pharmacy is of little to no risk to the health system.
Minimizing the burden of opening a 340B specialty pharmacy
We take the burden of opening a specialty pharmacy off your health system. We navigate you through the process of getting your specialty pharmacy running and successful. We handle the accreditation requirements. We get you access to the medications you need. We get you access to the payors.
Clinically integrating your 340B specialty pharmacy
We also take responsibility for integrating your specialty pharmacy with your clinic teams. Then we take-on everything that's required to grow your specialty pharmacy. We get to know your doctors, your clinicians, and your patients — so that we can tailor your specialty pharmacy’s services and medications to the needs of your patients, and the difficult disease states that your health system needs to manage.
340B specialty pharmacy accreditation: A VERY brief overview
Our Specialty Pharmacy team follows a comprehensive To Do list it manages — and personally undertakes — in guiding 340B health systems through the process of earning specialty pharmacy accreditation. Below is you’ll find just six of the twelve steps we take in the first of nine separate stages to earn specialty pharmacy accreditation:
- Create a call center function. (Customized according to your specific goals).
- Develop Key Performance Indicators and reporting metrics for all relevant stakeholders. These services may be performed either virtually or in-person at your facilities and/or clinics.
- Establish call center services for managing your prescription orders, refill requests, medication related questions, and other calls.
- Evaluate your PBM for available Specialty Pharmacy benefits.
- Obtain prior authorizations under your health insurance benefit plans, or other Specialty Pharmacy plans.
- Implement and manage financial assistance programs for your indigent or uninsured patients.
Stage Two of our Nine Stage process involves no less than 12 primary steps, with 39 separate “sub-steps” spread-out across those 12 primary steps. And it goes without saying, every stage in process requires highly-specialized expertise; the kind of expertise that only comes from highly-specialized training, and hands-on experience.
Reaping the benefits of 340B specialty pharmacy compliance
The payoff to confirming your compliance with manufacturers’ protocols is twofold: 1) You’ll get reimbursed for the specialty drugs you’ve filled, and 2) Your pharmacy will get access to more specialty drugs from the manufacturers.
ADDITIONAL READING
So You Want To Build A 340B Specialty Pharmacy. How Hard Can It Be?
How Recent 340B Changes Impact Specialty Pharmacies In 2025
The evolving legal and legislative landscape surrounding the 340B Drug Pricing Program has significant implications for hospitals' specialty pharmacies. Here's a breakdown of the new developments and their likely impacts:
1. 340B contract pharmacy restrictions
Drug manufacturers have increasingly restricted the use of contract pharmacies, especially specialty pharmacies, arguing that the 340B statute does not require them to deliver drugs to multiple contract pharmacies. Ongoing litigation has created a significant amount of uncertainty for 340B entities.
Impact of contract pharmacy restrictions on 340B hospitals:
REVENUE PRESSURE: Specialty pharmacies operated by, or affiliated with, hospitals may lose access to 340B discounts if manufacturers prevail in restricting contract pharmacy arrangements.
REDUCED COST SAVINGS: Hospitals often rely on specialty pharmacy revenue to support uncompensated care. Unchecked manufacturer restrictions reduce margin opportunities from discounted drugs.
2. Court decisions and legal precedents
Litigation over HRSA's authority to enforce contract pharmacy arrangements is central to the current landscape.
Two Key 340B legal cases:
1) Sanofi v. HHS (2023)
Court: U.S. Court of Appeals for the Third Circuit
In this case, the court ruled in favor of Sanofi and the drug manufacturers, finding that the 340B statute is silent on the use of contract pharmacies.
2) AstraZeneca v. HHS (D. Del. and 3rd Cir.)
Courts: Delaware District & The U.S. Court of Appeals for the Third Circuit
AstraZeneca similarly challenged HHS’s interpretation of the 340B statute in this case. The District of Delaware sided with HHS, but was reversed on appeal.
Potential Impact on 340B Entities
These two rulings have already had significant consequences for many 340B-covered entities:
- Reduced Access to 340B Savings
- Increased Administrative Burden
- Service Reductions
- Lower 340B savings could force hospitals and clinics to scale back charity care, outreach programs or specialty services.
- Legal Uncertainty
- Increased Scrutiny
- Regardless of court rulings, the spotlight on 340B program integrity means hospitals must tighten eligibility and documentation controls.
3. HRSA 340B enforcement shifts
The Health Resources and Services Administration (HRSA) has taken varying stances on 340B enforcement due to the legal challenges and changes in administration policy.
Impact on 340B hospitals:
- Compliance Burden: 340B entities must navigate a shifting regulatory environment, including stricter audits and data tracking.
- Uncertainty in Planning: Legal ambiguity forces hospital systems to be overly cautious in optimizing their 340B programs.
4. State-level 340B legal actions
Numerous states have passed laws to protect 340B-covered entities and their contract pharmacies, leading to further legal conflicts with drug manufacturers. Altogether, eleven states have either enacted 340B protection laws or passed legislation protecting 340B health systems in at least one chamber of their state legislatures, while 15 more states have introduced similar bills.
Impact on 340B hospitals:
- Patchwork Compliance: Hospitals operating across multiple states must navigate differing rules regarding specialty pharmacy operations and 340B usage.
- Potential Relief: In supportive states, hospitals should be able to maintain access to 340B pricing through specialty pharmacies.
5. Direct manufacturer distribution models
Under this model, drug manufacturers ship medications directly to the covered entities (or their contract pharmacies) rather than through traditional wholesalers. The problem, of course, is that this places distribution in the hands of the very entities seeking to undermine the 340B program wherever possible.
6. Technology and 340b data transparency demands
Legal and regulatory scrutiny is prompting demands for better tracking of 340B drug use and patient eligibility. Given the ever-increasing complexity involved in dealing with manufacturer restrictions, and the 340B program itself, the need for customized, analytics-driven technology has never been more critical to optimizing prescription savings opportunities.
At the same time, the need for seasoned experts managing your software, your 340B program and your specialty pharmacy has never been greater.
For Further Reading:
Empower Your Health System’s 340B Program With Analytics
Specialized Software Can Only Do So Much For 340B Programs
Specific examples impacting 340b hospitals. Recommended responses.
1. Manufacturer policies and restrictions
RESPONSE: In addition to taking necessary actions to overcome manufacturer restrictions, many hospitals are litigating or joining amicus briefs supporting HRSA’s enforcement of their legal rights to 340B discounts.
2. Compliance and operational strategy
RESPONSE: Hospitals with in-house specialty pharmacies are in a stronger position than those using contract specialty pharmacies — both with compliance and operational strategy — but it’s critical to stay proactive. One tactic for defending your program during audits or legal scrutiny is taking steps to improve Patient-Centered Services, demonstrating that your specialty pharmacy provides improved adherence, a lower total cost of care, and better outcomes — all of which supports the 340B law’s intent.
WANT OUR RESOURCE GUIDE
IN DOWNLOADABLE PDF?
Chapter 7: 340B’s Outlook Moving Forward, And How To Prepare Your Program.
LAST UPDATED: 11.18.25
What the changing 340B landscape means for your health system.
The 340B landscape continues to evolve rapidly, and most 340B hospitals continue losing substantial amounts of money to drug manufacturer restrictions. These losses have forced many safety-net hospitals to cut back on services, making it even harder for underserved patients and communities to access affordable medications and critical healthcare programs.
Aside from manufacturer restrictions, the 340B program faces additional new challenges — and opportunities — driven by legislative updates, market dynamics and emerging technologies.
HRSA’s Rebate Model Pilot Program
As we mentioned at the very top of this page, HRSA’s 2026 Rebate Model Pilot Program, first introduced publicly July 31, is a program which — if expanded to include all 340B-eligible prescriptions — could literally have a catastrophic impact on every participating 340B health system’s finances, moving forward. Here’s why
Section 340B of the Public Health Service Act requires manufacturers to “offer” covered entities a price no higher than the 340B ceiling price at the time of purchase.
HRSA’s rebate model flips the order on its head: Under the Pilot Program, 340B hospitals will be forced pay, up front, Wholesale Acquisition Cost (WAC) — which is often double or triple the 340B ceiling — and only later (if all documentation and claims are accepted) will they receive their lawfully-entitled 340B-replenishment rebates.
Although the Pilot Program covers only the 10 drugs below, it’s been estimated that the annual 340B reimbursements for these drugs alone ranges from $6.3 billion to $12.5 billion. With some 2700 hospitals participating in 340B, that averages-out to an annual cash-flow burden of more than $2.340B million to nearly $4.67 million per hospital. Which means, strictly calculating on the average numbers, in any given month, your health system’s cash flow could be down by as much as $388,888 — while you wait for replenishment from drug manufacturers you hope will honor the program’s 30-day reimbursement period.
Drugs in HRSA’s Model Pilot Program:
Eliquis
Jardiance
Xarelto
Januvia
Farxiga
Entresto
Enbrel
Imbruvica
Stelara
Fiasp and related products: Fiasp FlexTouch, Fiasp PenFill
NovoLog and related products: NovoLog FlexPen, NovoLog PenFill
What VytlOne is doing to prepare the 340B health systems we serve
340B health systems with on-campus pharmacies should expect a preliminary financial impact assessment for those pharmacies. Which is why we’ve taken the following preparatory steps:
- Assembled cross-functional team of experts across operations, 340B, finance, and technology.
- Assessing financial and operational impacts for each pharmacy.
We’ll also be offering a new service, 340Bridge.
340Bridge is a market-competitive, short-term loan designed to meet this moment by reducing health systems’ working capital exposure due to the 340B discount-to-rebate changes.
Additional support we’ll be offering
- Assessing pharmacy workflow and dispense platforms (e.g., GuardianRx) to support updated workflows and reporting requirements.
- Coordinating with the 340B program’s many stakeholders — including wholesalers, 340B TPAs and Beacon — to streamline communications and processes.
- Determining the best approach to register, submit data, and reconcile payments for 340B Rebate (i.e., Beacon) and Medicare’s Maximum Fair Price (MFP) Rebate.

Bausch Pulls Its Drug Catalog From The 340B Program.
NOTE: The following is a highly-condensed version of our in-depth article / editorial exploring the Bausch issue.
Bausch Health (BHC) shocked many healthcare industry observers when it publicly declared its intention to cease participation in the Medicaid Drug Rebate Program and the 340B Drug Pricing Program effective October 1, 2025.
In a statement published on its own website, the company claims, Bausch Health remains committed to Medicaid patients who have been prescribed our products and maintaining patient care and ensuring continuity of treatment is important.
How about Bausch’s commitment to 340B hospitals & patients?
By withdrawing its drugs from the 340B program, BHC is reducing access to a critical source of support for financially-struggling 340B hospitals, and for the patients they serve.
Is Bausch surrendering its Medicare Part B reimbursements?
Legally, participating in the 340B program is optional only insofar as the company not participating forfeits the right to have its drugs covered by Medicare Part B — which represents an estimated 27% of all Medicare reimbursements.
We have to wonder if BHS’s legal team has devised what they believe is a strategy for eliminating 340B obligations while still qualifying for Medicare Part B reimbursements. That said, there seems to be some uncertainty about BHC’s intentions in withdrawing from the 340B program. Company verbiage indicates BHC does not intend to withdraw every single product from 340B pricing. However, the 340B law as written is clear: You’re either all-in, or all-out.
The PPA and Medicaid Program participation
The Pharmaceutical Pricing Agreement (PPA) is a contract between drug manufacturers and Health and Human Services (HHS), and is a prerequisite for participation in the Medicaid Program and the 340B Drug Discount Program. BHS never signed the PPA.
What does this mean for 340B hospitals & patients?
Presumably, it means many patients will be forced to buy prescriptions direct from Bausch without insurance. What about hospitals who count-on 340B savings to help them stay afloat? Those hospitals will now be required to pay either Wholesale Acquisition Costs (WAC) or Group Purchasing Organization (GPO) prices — both which are significantly higher than 340B costs.
Will other manufacturers follow Bausch’s lead?
This, of course, is the most far-reaching question for, and threat to, the future of the 340B program and the health systems who depend on it.
Most discouraging of all is HRSA’s continued failure to enforce the 340B law as written — not to mention its own 2021 concession that it has no real power to enforce 340B program guidelines.
The good news for 340B entities
Despite the hundreds, if not thousands, of individual 340B manufacturer restrictions thrown our way, VytlOne continues to generate substantial savings and revenues for the health systems we serve. Which is why we remain optimistic that the 340B program will survive this latest attack.
VytlOne is here to help.
To learn how VytlOne can help your health system succeed in an ever-changing 340B environment, contact Howard Hall.
howard.hall@VytlOne.com | 214.808.2700
Navigating 340B Program Changes
Maximizing pharmacy’s role in your hospital’s revenue cycle
As mentioned in a previous chapter, VytlOne has supported the 340B programs of 33 health systems and 38 health centers since 2019. Altogether, we’ve generated nearly $1 billion in pharmacy-related savings for our clients. Moreover, despite drug manufacturer restrictions that have devastated many hospitals’ programs, every one of the health systems whose 340B programs we manage has enjoyed significant 340B-revenue increases.
The sad truth is that most 340B hospitals are struggling to protect their programs from further prescription-savings erosion — which is particularly unfortunate, given the fact that the hospitals we serve are often asking themselves how they can further optimize their 340B savings. All of which is why the ultimate question for a 340B-eligible entity might be: Which group is your hospital in: The former, or the latter?
Breakthrough: A PBM just for 340B hospitals
With VytlOne's PBM, health system pharmacies (retail and specialty) get prescription drugs on a pricing basis that’s similar to the cost-plus model. The hospitals we serve have the ability to design their own formularies and networks. They determine the margins their pharmacies generate on prescriptions, ensuring they operate on a positive-revenue basis — while enabling them to 1) drive the lowest possible costs for patient prescriptions, and 2) pass-along lower prescription costs to their employees.
Full transparency plus pricing and patient-care control for your hospital.
When VytlOne also manages your 340B program, your providers can choose — on a per-prescription basis — whether to take the associated rebate price of a drug or the discounted 340B price on each 340B-eligible prescription. Not only does your hospital benefit from lower pricing, you benefit from the full transparency we offer you on every prescription.
By having full access to pricing information, your pharmacists and providers can select the best prescription for each patient individually.In short, you ensure maximum clinical benefit for your patients and the highest possible revenue benefit for your 340B health system.
You can even extend savings to your employees.
With your prescription drug savings, you could easily cover the copay of every employee prescription filled in your pharmacies, and still increase your margins. Using the additional remaining margins, you can invest even further in caring for the community’s most vulnerable patients.
Think of the positive impact you could have on employees’ sense of well-being, their job satisfaction and their motivation to perform, by covering 100% of their prescription copays. Think of the positive impact that could have on your patients.
To learn more, contact Howard Hall: howard.hall@vytlone.com | 214.808.2700
Understanding the current 340B landscape
Key changes either anticipated or already implemented include:
Heightened 340B audits and oversight
The Health Resources and Services Administration (HRSA) has signaled its intention to increase the number and complexity of 340B program audits it conducts.
A new drug manufacturer ploy to undermine 340B
Manufacturers continue to challenge virtually every aspect of the 340B program, from drug pricing to contract pharmacy arrangements. One of the latest ploys they’ve pulled out of their bag of tricks is a so-called “Rebate Model” for 340B pricing.
“In a nutshell,” says VytlOne VP Heather Brooks, “the CE would have to pay retail prices first to allow for replenishment and THEN submit documentation like they do for 340B ESP (this time with even more claims info). Then the manufacturer will approve a ‘rebate’ and send money back to the CE for the difference in the 340B and retail prices. This effectively turns the entire 340B process on its head. Manufacturers are now asking already-starved nonprofit hospitals to pay significantly more upfront, with only the hope of receiving timely rebate payments. The Department of Health and Human Services (HHS) has put its foot down to stop this, and the manufacturers who’ve tried it — including Johnson & Johnson, Bristol Myers Squibb, Lilly and Sanofi — have all placed the maneuver on hold.”
Dirty tricks from who knows where
Someone is authoring false reports and smear campaigns to undermine the 340B program in the court of public opinion. The Kentucky Lantern, an independent news service, reported that a ‘dark money’ group has claimed the 340B program is being used to subsidize health care for illegal immigrants and pay for gender transition for kids. Another myth being spread is that the money supporting the 340B program comes out of taxpayers’ pockets.
340B legislative updates: States opposing manufacturer restrictions
More states are enacting 340B protection bills. As we mentioned in a previous chapter, eleven states have either enacted 340B protection laws or passed legislation protecting 340B health systems in at least one chamber of their state legislatures, while 15 more states have introduced similar bills.
Few manufacturers have officially abandoned their restrictive practices completely, but now the states have firepower to answer them. “In states where the laws have been in place the longest,” says Brooks, “we’re seeing significantly more savings generated for their programs. For one of our clients, we were able to increase one pharmacy chain’s monthly 340B reimbursements from less than $10,000 to more than $100,000 a month.”
MAY, 2025 UPDATE: Executive Order 14297
On May 12, President Trump signed Executive Order 14297 — which could significantly impact the 340B Drug Pricing Program.
Key Implications for 340B Reimbursements
- Potential Reinstatement of Medicare Reimbursement Cuts
- Introduction of 'Site Neutrality' Payment Models
This approach could lower reimbursements for hospital outpatient departments to match those of non-hospital facilities, potentially diminishing the 340B program’s financial benefits for hospitals. - Emphasis on Transparency and Direct Patient Discounts
This includes proposals requiring PBMs and pharmacies to pass drug discounts directly to patients at the point of sale. Such measures could transform the 340B program into a patient entitlement system, potentially impacting the financial viability of safety-net providers. - Implementation of 'Most Favored Nation' Pricing
The goal here is to align U.S. drug prices with those in other developed countries. This could lead to significant reductions in drug prices, and decrease 340B margins.
340B Pharmacy Network Adjustments
Restrictions on contract pharmacy participation remains a hot-button issue, not to mention a central focus of unlawful manufacturer 340B program restrictions. Based on our experience, here is a claim we can make with 100% certainty: Your hospital’s 340B contract pharmacy network is not what it should be. To learn what you can do to expand and optimize it, click here.
Key Strategies for 340B Compliance
Strengthen your internal policies and procedures
Enhance your documentation practices
Engage in proactive communications with 340B program stakeholders
The Expanding Challenges of 340B in 2025
1. Manufacturer restrictions: The battle continues
Many drug manufacturers have doubled down on restrictive policies that limit covered entities’ ability to access 340B pricing.
2. HRSA enforcement: Limited but persistent
While HRSA has attempted enforce 340B rules, the reality is that covered entities must take proactive measures to secure their savings.
3. TPAs and contract pharmacy networks: The need for optimization
Not all TPAs are created equal. For tips on selecting the right TPAs for your 340B program, click here.
How 340B Entities Can Optimize Their Program Benefits
1. Advanced 340B software & automated analytics
VytlOne’s proprietary analytics software automates data tracking, ensuring that covered entities can efficiently manage their savings opportunities while maintaining strict 340B program compliance.
2. Full-time, expert 340B program management
Far too many health systems rely on part-time staff, with no outside support, to manage their 340B programs. That’s never worked, and it never will.
3. Overcoming manufacturer restrictions with proven strategies
The challenge of overcoming manufacturer restrictions is constantly evolving, and requires a combination of analytics and human insight. To learn more about striking the right balance between the two, click here.
4. Getting the most from your contract pharmacies
Earlier we discussed the importance of health systems expanding their contract pharmacy networks. For more information on evaluating your existing contract pharmacies, click here.
5. Build your own retail & specialty pharmacies
On average, retail pharmacies managed by VytlOne generate $750 to $1,000 in net profit per hospital bed, per month. Specialty pharmacies can generate as much as six times more 340B revenue than traditional retail pharmacies. To learn how your health system can fund and manage successful on-campus pharmacies, click here.
6. Use your 340B savings to expand patient services
To learn more about how two of the systems we support have done just that, click here.
Qualities Common To Successful 340B Programs
A solid understanding of 340B program benefits
Launching and maintaining a successful 340B program starts with your health system truly understanding 340B’s savings and revenue potential — and, in turn, the potential of your 340B income to positively impact patient outcomes, not to mention your system’s overall mission in the community you serve.
A system-wide culture of 340B program support
“The hospitals who benefit the most from working with us,” says Brooks, “are the ones who are willing to collaborate with us, and recognize that they can trust us. We do the vast majority of the work, but we still need their support — particularly in responding to our team’s data requests.”
A commitment to optimizing 340B clinical opportunities
“It’s no secret that some covered entities have more existing 340B opportunities than others,” she continues, “because they have more 340B-compatible clinical programs. We’ve helped number of health systems add clinical programs that can serve new 340B-eligible patients.”
“Ultimately,” Brooks concludes, “what gives me the greatest job satisfaction from serving health systems’ 340B programs is my ability to positively impact their missions. I consider myself to be more than just a partner of those hospitals. In a very real sense, I’m an extension of their missions.”
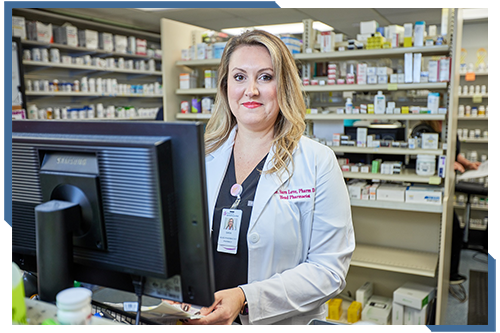
VytlOne is here to help, if you have questions.
There are so many ways to optimize your 340B drug program savings and benefits — overcoming manufacturer restrictions while maintaining compliance at all times. For more information on any aspect of developing and managing a successful 340B program, contact Howard Hall. C: 214.808.2700 | howard.hall@vytlone.com
Chapter 8: Frequently Asked 340B Questions.
What is the purpose and intent of the 340B Drug Pricing Program?
1. Stretch scarce health-care resources
Congress created the 340B Program in 1992 to strengthen health systems serving vulnerable populations, allowing eligible safety-net providers to purchase outpatient prescription drugs at significantly discounted prices — thereby enabling them to:
- Reduce the cost of drugs for uninsured and underinsured patients
- Expand access to needed services
- Improve health outcomes in underserved communities
2. Support and stabilize the safety-net
The 340B program is also designed to ensure that hospitals and clinics caring for large numbers of low-income or rural patients remain financially viable. The savings allow covered entities to:
- Offer sliding-scale or charity care
- Fund patient support programs (transportation, care coordination, language services, adherence programs, etc.)
- Maintain services that otherwise operate at a loss (oncology, HIV clinics, rural clinics)
The intent is to stabilize the health-care safety net that low-income patients rely on. In plain terms, the 340B Program exists to help safety-net providers do more with limited resources, so patients who face financial, geographic or social barriers can access the medications and services they need.
Which types of health systems and facilities qualify for 340B eligibility?
1. Hospitals (government-owned, government-operated, or have government contract for serving low-income patients)
Hospitals must also meet a Medicare Disproportionate Share Hospital (DSH) threshold and cannot obtain group purchasing organization (GPO) drugs unless exempt. Eligible hospital types include:
- Disproportionate Share Hospitals (DSHs)
- Children’s Hospitals (PEDs)
- Critical Access Hospitals (CAHs)
- Rural Referral Centers (RRCs)
- Sole Community Hospitals (SCHs)
- Free-standing Cancer Hospitals (CANs)
2. Federal Grantee Organizations
These facilities qualify because they receive federal grants tied directly to serving vulnerable or underserved populations. Examples include:
- Federally Qualified Health Centers (FQHCs) / FQHC Look-Alikes
- Ryan White HIV/AIDS Program clinics
- Family planning clinics (Title X)
- Black Lung clinics
- Hemophilia Treatment Centers
- Native Hawaiian Health Centers
- Urban Indian Organizations
- STD and TB clinics
- Comprehensive Hemophilia Diagnostic and Treatment Centers
NOTE: Each grantee organization’s eligibility is tied to the specific federal grant under which it is funded.
3. Child Sites (“Offsite Facilities”)
- Hospitals and grantee organizations may extend 340B eligibility to certain outpatient clinics they operate if:
- The clinic appears as a reimbursable site on the parent organization’s Medicare Cost Report,
- It is listed under the correct cost center(s), and HRSA has approved it during 340B registration.
These are often referred to as child sites or offsite outpatient departments.
In short, 340B-eligible entities generally fall into two categories:
- Hospitals with safety-net characteristics (DSH, CAH, rural, children’s, cancer)
- Federal grantees serving underserved populations (FQHCs, Ryan White, Title X, etc.)
Together, these organizations form the backbone of the health-care safety net the 340B Program is intended to support.
What is the typical ROI or financial benefit of 340B participation?
1. Discount Levels
340B discounts typically reduce drug acquisition costs by:
- 25% to 50% on average
- Up to 60% or more for certain high-cost specialty drugs
These discounts translate directly into margin gains when drugs are dispensed to eligible patients.
2. Annual Financial Benefit (Typical Ranges)
Because 340B impact depends on size, payer mix, specialty services and contract pharmacy activity, the common ranges look like this:
- Small rural or CAH hospitals: ~$500,000 to $3 million per year
- Mid-sized community hospitals: $5 million to $10+ million per year
- Large DSH or academic hospitals: $20 million to $50+ million per year
- Federal grantee organizations (FQHCs, Ryan White clinics, etc.)
- FQHCs: ~$250,000 to $2 million annually
- Ryan White clinics: ~$1 million to $8 million, depending on HIV volume and specialty pharmacy utilization
3. ROI Compared to Program Costs
Most organizations experience ROI of 6:1 to 15:1. The operational costs of a well-run, compliant 340B program are relatively modest compared with the scale of savings and revenue generated — making it one of the most financially efficient tools available to safety-net providers.
4. Financial Benefits Beyond Direct Savings
In addition to margins on outpatient drugs, 340B savings can fund:
- Free or low-cost medications
- Care coordination and case management
- Patient transportation, translation and adherence support
- Expanded service lines (IE: Oncology, HIV care, behavioral health)
- Clinics that operate at a loss, but are vital for community access
These expanded services often yield far more critical Returns On Investment, including:
- Increased patient retention
- Improved patient outcomes
- Reduced uncompensated care
- Overall improved community health
NOTE: Every 340B health system served by VytlOne invests its program savings and revenue in achieving those returns. It’s why we agreed to serve them.
How can 340B savings be reinvested to improve patient access and community health?
340B savings can be reinvested in a wide range of programs and services that directly strengthen patient access, affordability and overall community health — expanding care for vulnerable populations in ways that would not otherwise be financially possible, including:
1. Reducing medication costs for patients
- Providing free or low-cost prescriptions for uninsured or underinsured patients
- Offering sliding-scale pricing or medication assistance programs
- Covering copays for patients who otherwise would not fill their prescriptions
This directly improves medication adherence and chronic disease control, while reducing the likelihood of preventable (and costly) patient readmissions.
2. Expanding access to essential health services
340B funds often support clinics and services that operate at thin or negative margins, such as:
- Oncology, HIV care, behavioral health and infusion services
- Rural clinics and satellite sites
- Pharmacy-led clinical programs (MTM, chronic disease management)
These expansions also make it possible for a community’s most vulnerable patients to receive care locally rather than traveling long distances. At the same time, they enable 340B hospitals to control healthcare quality by keeping the entire continuum of care within the health systems themselves.
3. Supporting care coordination and wraparound services
Many safety-net organizations use 340B savings to address non-medical barriers to care, such as:
- Care management and social work support
- Transportation to medical appointments and pharmacies
- Patient education, adherence counseling, and language services
- Case management for complex or high-risk patients
These services help prevent unnecessary hospitalizations and improve patient outcomes.
4. Improving health equity and preventive care
Savings often fund programs targeting high-risk or underserved populations, such as:
- Community vaccination campaigns
- Mobile clinics or outreach vans
- Screening and early-detection initiatives
- Chronic disease programs for diabetes, hypertension, and asthma
These initiatives directly reduce disparities in care access and outcomes.
5. Strengthening the financial stability of safety-net providers
While indirect, this benefit is critical for community health. 340B savings help:
- Offset uncompensated and charity care
- Maintain services in rural or low-income areas that would otherwise close
- Ensure long-term sustainability of safety-net hospitals and clinics
Stable providers mean sustained, and improved, access for the populations that rely on them most — reducing barriers to care, and strengthening the overall health of the providers’ communities.
What are the best practices for optimizing 340B savings while maintaining full compliance?
1. Strengthen eligibility tracking and documentation
GOAL: Prevent diversion and ensure every dispensed drug meets patient eligibility rules.
2. Maintain strict prescriber and location validation
GOAL: Avoid prescriptions written or filled from non-qualified locations or providers.
3. Leverage customized 340B software for mixed-use and split-billing
GOAL: Maximize capture of 340B-eligible dispenses while maintaining auditable inventory integrity.
4. Implement a robust internal audit program
GOAL: Identify issues early, correct them quickly, and prepare for HRSA or manufacturer 340B audits.
5. Strengthen Medicaid and managed Medicaid duplicate-discount protections
GOAL: Prevent the most common HRSA 340B-audit finding.
6. Establish carefully managed 340B contract pharmacy arrangements
GOAL: Expand 340B savings through retail and specialty channels without exposing your health system to compliance risk.
7. Develop clear, documented 340B policies and procedures (P&Ps)
GOAL: P&Ps should match operational reality. HRSA will check.
8. Train staff regularly
GOAL: Reduce errors and create a culture of 340B compliance.
9. Coordinate pharmacy, finance, compliance and IT teams
GOAL: Integrate compliance with operational and financial optimization.
10. Track and report how 340B savings are reinvested
While not required by statute, documenting 340B savings and their community impact is now considered an essential best practice.
GOAL: Demonstrate the program’s value and defend ongoing participation.
IN SHORT, The best way to optimize 340B savings while maintaining full compliance is to use strong eligibility and prescriber validation, automated split-billing tools, routine internal audits, strict Medicaid duplicate-discount protections, transparent contract pharmacy oversight, accurate policies and procedures and ongoing staff training. This ensures maximum savings with minimum compliance risk.
Download Our Free 2025 Compliance Checklist PDF
How can I minimize losses from manufacturer restrictions and 340B ESP data challenges?
1. Maximize capture at in-house pharmacies and onsite specialty pharmacies
Since the most punitive manufacturer restrictions affect contract pharmacies, the strongest mitigation strategy is to shift eligible prescriptions to onsite retail pharmacies.
2. Improve your 340B contract pharmacy network efficiency
In short, you should prioritize high-performing pharmacies and focus on specialty drug capture, where the margins — and the losses from restrictions — are highest.
3. Strengthen your prescriber-location mapping
Many manufacturer restrictions hinge on prescriber and location validation. Accurate mapping allows more claims to qualify, even within restricted rules.
4. Ensure accurate and timely data submission to 340B ESP
Although 340B ESP is burdensome, errors are costly. Improved submission quality correlates directly with higher claim approvals.
5. Advocate for replenishment through eligible prescribers
Many restrictions allow 340B pricing only when the prescriber is associated with a registered child site. Better 340B data integrity means fewer denied replenishments.
6. Use real-time data to identify suppressed or rejected claims
This allows targeted mitigation, such as shifting patients, prescribers or pharmacy routing.
7. Expand eligible service lines tied to high-value savings
Growth in outpatient services can offset restriction losses, while higher outpatient volume increases the pool of eligible 340B prescriptions — even when restrictions tighten.
8. Strengthen patient adherence and retention programs
Better patient retention increases refill capture and mitigates lost 340B margins from limited capture elsewhere.
9. Work with TPAs and wholesalers for exception handling
Some manufacturers allow exceptions for rural providers, providers with no in-house pharmacy and certain specialty medications. Coordinating with your TPA(s) and wholesaler(s) ensures you're taking advantage of exception pathways when eligible.
10. Build a clear internal financial model to quantify 340B losses
By calculating lost 340B savings by manufacturer, pharmacy and ESP-related denial rates, you can make data-driven decisions on everything from network optimization and patient routing and prescriber alignment to whether you should challenge or escalate issues with manufacturers or vendors. This also strengthens your ability to defend the program to leadership.
FOR FURTHER READING:
Overcome 340B Restrictions With Software And Human Insight
Six Prescription-Reporting Errors To Avoid In 340B ESP
Optimize 340B Program Savings & Compliance With Data Mining

VytlOne is here to help, if you have questions.
There are so many ways to optimize your 340B drug program savings and benefits — overcoming manufacturer restrictions while maintaining compliance at all times. For more information on any aspect of developing and managing a successful 340B program, contact Howard Hall. C: 214.808.2700 | howard.hall@vytlone.com